This publication by Falletto et al. explores the benefits of using transanal irrigation for people with FBD and LARS, pointing to significant improvements in patient's quality LARS score during the study period.
Introduction to the study
Patients suffering from functional constipation (FC), functional faecal incontinence (FI), and low anterior resection syndrome (LARS) all share the unpleasant symptoms associated with bowel dysfunction. Condition-related symptoms as these have a major impact on an individual's quality of life (QoL), affecting them physically, psychologically, and socially. While Transanal Irrigation (TAI) is a well-established treatment option for patients with Neurogenic Bowel Dysfunction (NBD) (typically expressed in diseases such as Multiple Sclerosis and Parkinson's or following Spinal Cord Injury), there remains some question as to whether people with Functional Bowel Disorders (FBD) or LARS can benefit from TAI.
What is functional bowel disorder and LARS?
Functional bowel disorders refer to bowel dysfunction where no neurogenic or organic cause can be found. While the symptoms of FBD and NBD are the same (faecal incontinence, constipation, and incomplete emptying), the underlying cause is what differs them. Diagnosis and treatment of people with FBD is often considered more difficult and FBD patients tend to persevere with their problems longer than those with NBD. About 50% of adults who seek healthcare after more than 3 months of abdominal discomforts are diagnosed with FBD.
Low Anterior Resection Syndrome – LARS – is a constellation of symptoms or problems patients experience in varying degrees after rectal surgery. When undergoing surgery for rectal cancer, all or part of the rectum is removed and the end of the bowel and what is left of the rectum/anus are connected together. This junction is called an anastomosis. Depending on the location of the tumour, a high or low resection of the rectum is performed. The rectum functions as a container for stool, and once this function is removed it may lead to more frequent bowel movements and a sensation of incomplete emptying. Surgery, radiotherapy, and chemotherapy may also cause nerve damage, which may lead to impaired rectal sensation and increased difficulty feeling whether gas or stool is to be passed. It may also be difficult to keep the sphincter closed, leading to a risk of stool or gas leakage.
What is Transanal Irrigation?
Transanal irrigation is a minimally invasive and reversible treatment for bowel dysfunction which introduces a large volume of lukewarm water into the bowel via the anus and facilitates the emptying of the rectosigmoid and left colon. With this part of the bowels efficiently emptied it will take approximately 2 days until new faces reach the rectum, allowing the patient better control of when and where they empty their bowel, increasing independence and avoiding accidents.
With this multicentre observational study (12 centres; 369 patients), Falletto et al wanted to evaluate the level of satisfaction regarding bowel control and quality of life following short term (6 months) treatment with TAI. Furthermore, they looked to evaluate bowel symptoms severity and the dropout frequency and reason.
The 12 centres followed the same shared clinical protocol and used disorder specific validated questionnaires to assess patient QoL and efficacy of TAI at 1 and 6 months (results from 12 and 24 months are due to be published as a long-term study at a later stage). The protocol included patients meeting the following criteria: over 18-years of age, prescribed to use TAI as part of the normal clinical practice, not previously treated with TAI, trained to handle the irrigation system by healthcare professionals and consent to be included in this study.
Can transanal irrigation improve quality of life?
To evaluate the efficacy of TAI in the participants, the study protocol used bowel control satisfaction score evaluated using a visual analogue scale (VAS scale) ranging from 0 (not satisfied at all) to 10 (completely satisfied) as well as QoL scores evaluated using disorder specific validated questionnaires. From the analysis of the primary and secondary endpoints of the present study it can be concluded that patients suffering from FC, FI, and LARS benefit from short-term treatment with TAI. QoL, satisfaction regarding bowel control, and severity of disorder-related symptoms were substantially and significantly improved following a 6-month TAI treatment.
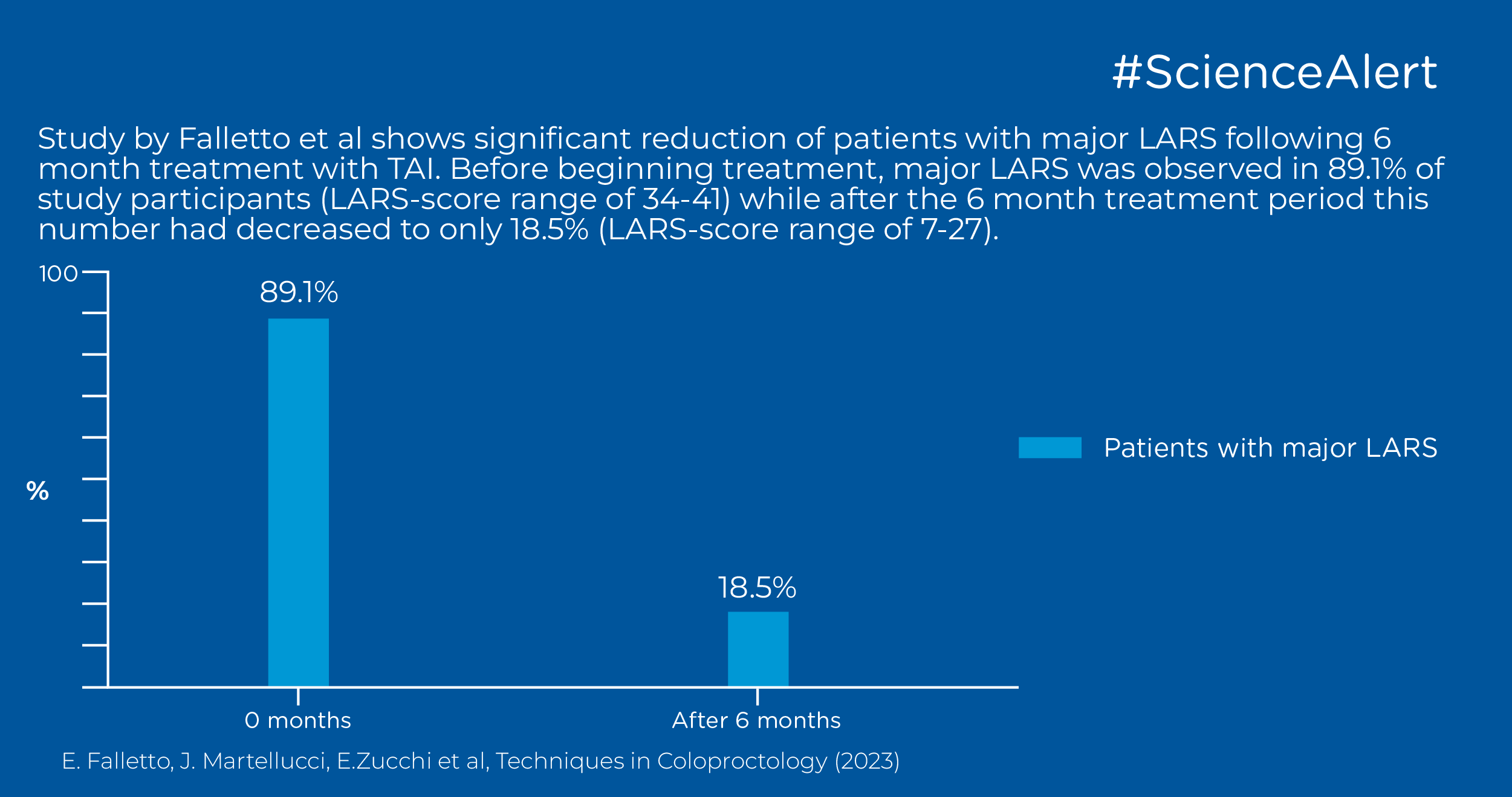
Can transanal irrigation lower LARS-score?
The severity of LARS varies between patients, from major LARS, to minor or no LARS. Prior to treatment with TAI, major LARS was observed in 89.1% of study participants (LARS-score range of 34-41) while after the 6 month treatment period this number had decreased to only 18.5% (LARS-score range of 7-27). The results in this study by Falletto et al are consistent with previous literature, such as in similar studies by Martellucci et al. and Enriquez-Navascues et al. who observed a drop of the disorder severity score from major LARS to no LARS, reporting median LARS score from pre-treatment values of 35.1 (range 30–42) and 35.0 (range 32–39) to post-treatment values of 12.2 (range 0–21) and 12.0 (range 12– 26), respectively.
Does patient selection for TAI matter?
One of the main challenges when initiating TAI is adherence to the therapy. It may take patients up to 12-weeks to properly adjust to the therapy and previous short-term studies have noted drop-out rates of between 18-23%. The dropout rates in this study were observed to be 8% which is notably lower than the data reported in literature. Falletto et al relate this result to specific patient selection, where TAI was not prescribed to patients who were able to properly perform or felt uncomfortable with the procedure, even after 1 month of trial. These results highlight the importance of a thorough and protracted training in a specialised centre, as most dropouts reported in the literature may be ascribed to the undesired effects encountered by incorrectly trained patients and thus adequate training may be the only factor that has a statistically significant impact on the risk of dropout and complication.
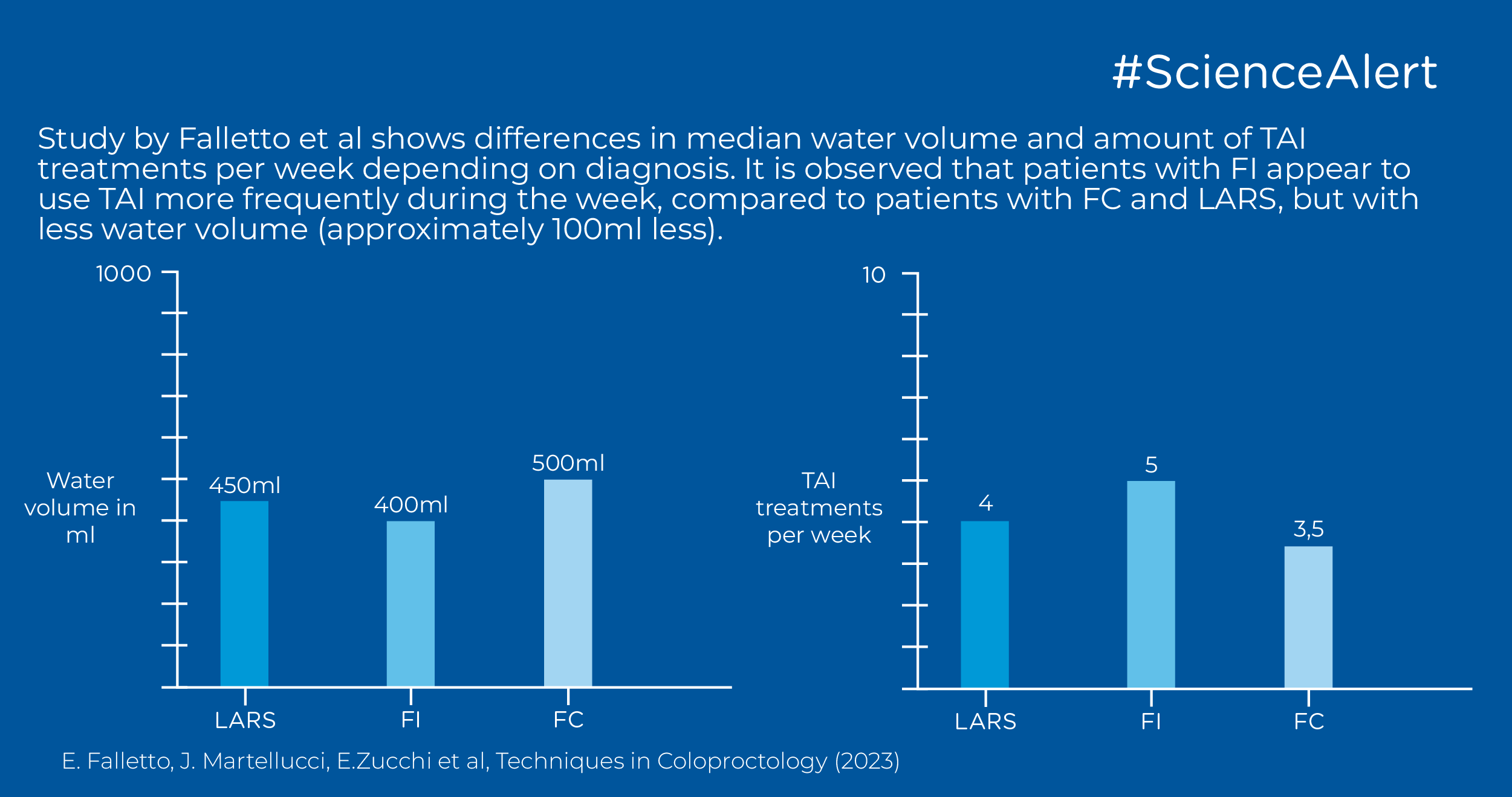
Does treatment frequency and water amount in TAI vary by disorder?
According to the results of this study, it is observed that patients with FI appear to use TAI more frequently during the week, compared to patients with FC and LARS, but with less water volume (approximately 100ml less). The median water volume for LARS patients was observed to be 450ml and median frequency for amount of TAI treatments performed per week at 4. This is line with previous literature as well. For FI and FC patients, the TAI frequency was noted to be 5 and 3.5 respectively which is also in line with previous literature. Median water volumes for FI and FC were at 400ml and 500ml respectively, which is slightly lower compared to previous studies.
Conclusions
Based on the data presented in this multicentre observational study by Falletto et al, it can be concluded that treatment with tranasanal irrigation is beneficial in the short term for patients who suffer from FBD and LARS. 6-month treatment with TAI enabled a significant improvement of QoL scores, satisfaction scores related to bowel control, and severity indexes of disorder-related symptoms in patients suffering from FC, FI and LARS. A future analysis of long-term data (up to 24 months) will follow, with focus on the clinical outcome of long-term treatment with TAI for patients dealing with FBD and LARS.